Ultrasound Scan of the Thyroid and Parathyroids
Ultrasound is a painless safe technology that uses sound waves to form an image of tissues. It is particularly good at looking at the thyroid gland. It provides a lot of detailed information about thyroid nodules. All patients with a thyroid nodule should have a thyroid ultrasound. Ultrasound is also very good at evaluating lymph nodes in the neck that may be involved with thyroid cancer.
Having an Ultrasound Scan of the Thyroid
An ultrasound scan of the thyroid is painless and quiet. It is best to wear an open neck shirt so that it is easy for the person doing the ultrasound scan to access your lower neck. You are asked to lie down on your back with your neck extended (tilting the head back). A cover is placed over the top of your shirt to help prevent any ultrasound gel going onto your clothes.
The gel is water soluble and does not stain clothes. Gel is placed on the skin of the lower neck and a transducer (flat probe) is placed on top the gel. No pressure is applied. The transducer is moved across the neck to look at different areas of the neck. Images are saved. No medications are given, so it is safe to drive home afterwards.
TIRADS Classification System
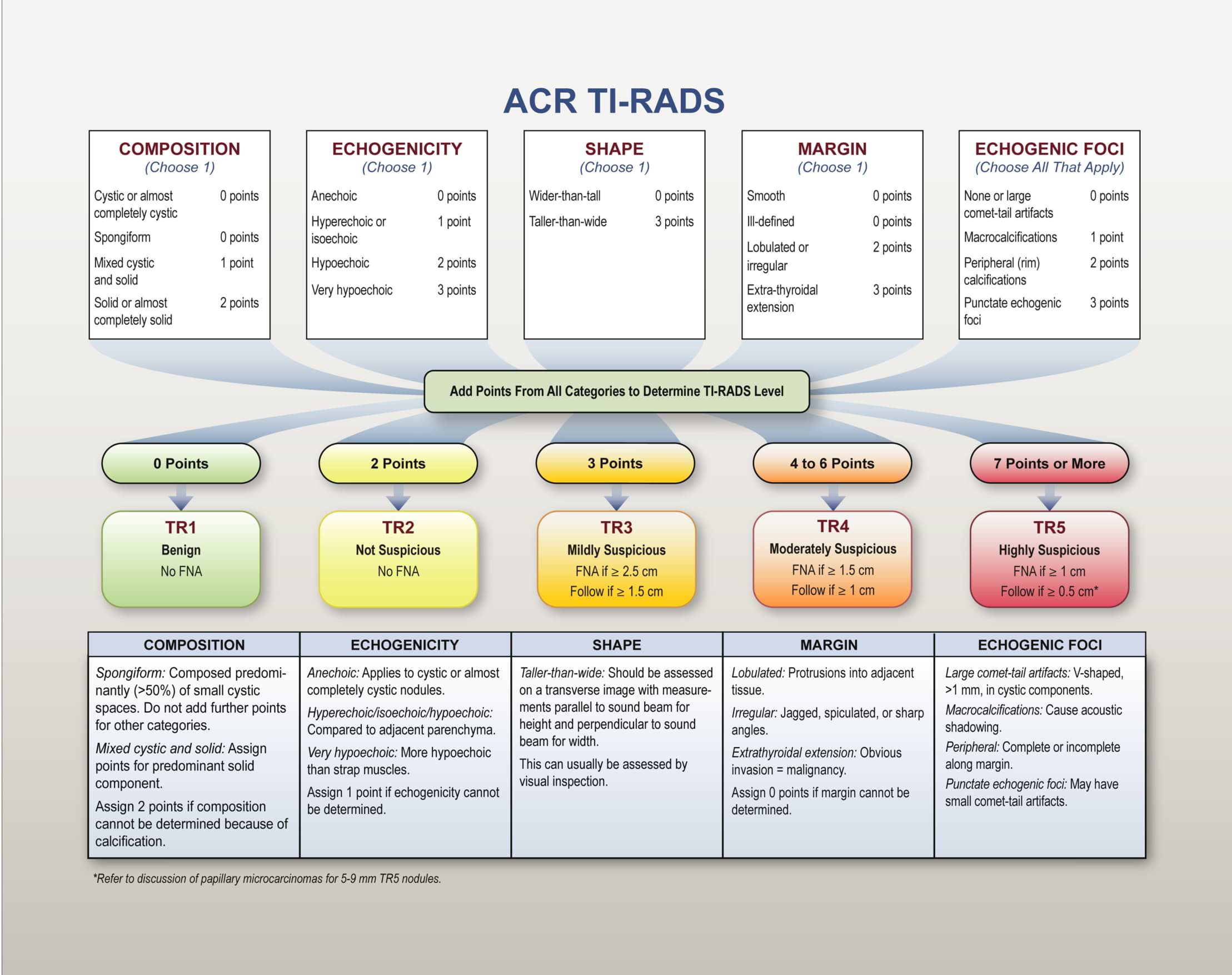
The dimensions and volume of your thyroid gland are calculated from the images obtained. The number, size, and location, of any thyroid nodules are noted. The American College of Radiologists developed the Tirads system (Thyroid Imaging and Data Systems) to classify nodules according to the following criteria (references 1, 2):
Composition (solid, cystic, ..)
Echogenicity (hypoechoic, isoechoic, ..)
Shape (wider than tall, taller than wide)
Margin (smooth, irregular, ..)
Echogenic foci (=calcifications): none, macrocalcifications, ..
Echogenicity refers to the darkness or lightness of the nodule in relation to the surrounding tissue. Points are given for each of these characteristics. The nodules are given an overall score between 1-5 according to the above criteria. This score predicts the risk of malignancy for that nodule. The higher the score the more likely the nodule is to be malignant.
ACR White paper 2017.
Recommendations are made depending on the size and Tirads classification.
For example,
- FNA is recommended for a 1.5cm Tirads 4 nodule,
- while ultrasound surveillance is recommended for a 2cm Tirads 3 nodule.
- A 4cm Tirads 2 nodule requires no follow up.
- It is important to remember that these recommendations are for asymptomatic euthyroid patients.
The risk of malignancy increases with a higher Tirads classification as follows:
| Tirads | Description | Risk of malignancy |
| 1 | benign | 0.3% |
| 2 | benign | 1.5% |
| 3 | Mildly suspicious for malignancy | 4.8% |
| 4 | Moderately suspicious for malignancy | 9.1% |
| 5 | Highly suspicious for malignancy | 35% |
Basically, the size and Tirads score determines which patients need FNA and which patients need ultrasound surveillance.
Ultrasound of Lymph Nodes
Ultrasound is also used to detect any abnormal looking lymph nodes that may be involved with thyroid cancer. The size, shape, and imaging characteristics of the lymph nodes, determine if they are involved with cancer (reference 4). The locations of any abnormal lymph nodes are noted. Ultrasound guided FNA is performed on any abnormal lymph nodes to confirm the presence of cancer.
Ultrasound of other Thyroid Pathologies
- Giraffe skin pattern. A thyroid with a giraffe skin pattern of appearance is sometimes seen with Hashimoto’s thyroiditis.
- Comet tails. An ultrasound appearance of comet tails is associated with a benign colloid cyst.
- Halo sign. A thin, hypoechoic rim around a nodule is associated with benign nodules.
- Thyroid inferno. The appearance of increased blood flow in the thyroid is seen in Grave’s disease.
- White knight. A well-defined white (hyperechoic) nodule without calcifications is sometimes seen in Hashimoto’s thyroiditis.
Parathyroid Ultrasound
Normal parathyroid glands are not usually visible on ultrasound. Enlarged parathyroid glands seen in hyperparathyroidism are frequently seen on ultrasound. Enlarged parathyroid glands are seen as hypoechoic (dark grey) masses adjacent to the thyroid gland.
Ultrasound is very useful to determine the position of an abnormal parathyroid gland and guide the surgeon to the correct location. Sometimes thyroid nodules and lymph nodes can be mistaken for parathyroid glands on ultrasound scanning.
Dr Hall and Ultrasound
Dr. Hall has been performing ultrasound, ultrasound guided FNA and ultrasound guided core needle biopsies since 2007. He has trained in ultrasound, attending courses and lectures, been a course director, taught ultrasound to junior doctors and colleagues, and also been on a review panel for ultrasound procedures. Dr Hall was the course director for a one-day ultrasound workshop at the New Zealand Society of Otolaryngology Head and Neck Surgery annual scientific conference in October 2024.
References:
- Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. (2017) Journal of the American College of Radiology : JACR. 14 (5): 587-595. doi:10.1016/j.jacr.2017.01.046 - Pubmed
- Grant EG, Tessler FN, Hoang JK, Langer JE, Beland MD, Berland LL, Cronan JJ, Desser TS, Frates MC, Hamper UM, Middleton WD, Reading CC, Scoutt LM, Stavros AT, Teefey SA. Thyroid Ultrasound Reporting Lexicon: White Paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. (2015) Journal of the American College of Radiology : JACR. 12 (12 Pt A): 1272-9. doi:10.1016/j.jacr.2015.07.011 - Pubmed
- Middleton WD, Teefey SA, Reading CC, et al. Multiinstitutional Analysis of Thyroid Nodule Risk Stratification Using the American College of Radiology Thyroid Imaging Reporting and Data System. (2017) American Journal of Roentgenology. 208 (6): 1331-1341. doi:10.2214/AJR.16.17613 - Pubmed
- Ahuja AT, Ying M, Ho SY, Antonio G, Lee VP, King AD, Wong KT. Ultrasound of malignant cervical nodes. Cancer Imaging 2008; 8:48-56.