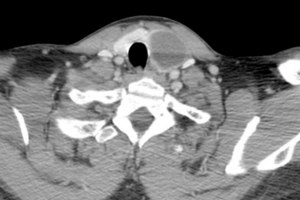
Thyroid cysts are common, and most are benign. Thyroid cysts may have a solid component and the solid component may be malignant. However pure thyroid cysts are seldom malignant. Thyroid cysts may be classified as:
Cystic > 90% cystic
Predominantly cystic: 50-90% cystic
Mixed: solid and cystic. Less than 50% cystic
Most thyroid cysts are formed from degenerating thyroid adenomas. Thyroid cysts may be solitary or multiple.
The basic unit of the thyroid is the thyroid follicle which comprising a sphere of thyroid follicular cells with colloid in the centre of the sphere. The thyroid follicular cells are cuboidal in shape and make thyroglobulin, T4 and T3. Colloid contains thyroglobulin, T4, T3, monoiodotyrosine (MIT) and diiodotyrosine (DIT). Thyroid stimulating hormone (TSH) not only stimulates the thyroid to produce T4 and T3 but also stimulates the thyroid follicular cells to grow.
Symptoms of Thyroid Cysts
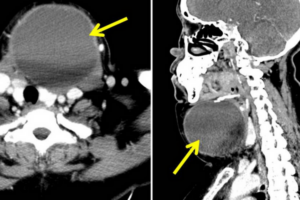
Thyroid cysts may be entirely asymptomatic. As they enlarge, they cause compressive type symptoms including a pressure feeling in the neck, globus symptoms-feeling of a lump in the throat. They may cause dysphagia, voice change or shortness of breath from compression of the trachea. Most patients with thyroid cysts are euthyroid. Patients may also simply complain of an unsightly lump in the lower neck.
Once the lump has reached a certain size it is usually obvious clinically and can be seen to move on swallowing. Despite being cystic it may feel either soft or firm.
Investigation
An ultrasound scan is the investigation of choice. Thyroid nodules are classified according to the tirads system. Cystic nodules are usually tirads 1 or 2 and as such do not require ultrasound guided FNA cytology. Comet tail artefacts may be seen on ultrasound scan and indicated a benign thyroid cyst. Tirads 3 nodules greater than 25mm, tirads 4 nodules greater than 15mm and tirads 5 nodules greater than 10mm all required ultrasound guided FNA cytology. As with all thyroid pathologies, thyroid function tests are also recommended.
Treatment
Patients with no symptoms and thyroid cysts classified as tirads 1 or 2 require no treatment. Patients with symptoms and a large thyroid cyst are best treated with ultrasound guided aspiration of the thyroid cyst. The cyst contents are sent for cytology but usually the report comes back as non diagnostic due to the low number of thyroid follicular cells present in the aspirate. About 80% of thyroid cysts recur after aspiration. However, 20% of patients are cured. If the thyroid cyst recurs, then ultrasound guided ethanol ablation of the thyroid cyst is recommended. This is a simple procedure with a high chance of cure. The expected volume reduction ratio for a cystic thyroid mass after ethanol ablation is 85%. If the cyst still recurs then further ethanol ablation should be considered. For patients with a solid component to the thyroid cyst, ultrasound guided FNA cytology is recommended. If FNAC is benign then radiofrequency ablation can be considered. Alternatively thyroid lobectomy (hemithyroidectomy) can be performed.
Summary of Treatment for Thyroid Cysts
- Asymptomatic: no treatment
- Tirads 3, 4, 5: ultrasound guided FNA depending on size.
- Simple aspiration under ultrasound guidance
- Ethanol ablation under ultrasound guidance
- Radiofrequency ablation under ultrasound guidance
- Thyroid lobectomy.
References:
- Grant EG, et al. Thyroid Ultrasound Reporting Lexicon: White Paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. J Am Coll Radiol 2015;12:1272-1279.
- Hahn SY, et al. Ethanol ablation of the thyroid nodules: 2018 consensus statement of the Korean Society of Thyroid Radiology. Korean J Radiol 2019;20(4):609-620.
- Maniam P, et al. Ethanol ablation for recurrent symptomatic thyroid cysts: 5-year UK-based experience. Clin Otol 2023;48:250-253.