A goitre is simply an enlarged thyroid gland. It is not a pathological diagnosis, just a descriptive term. A goitre is most commonly benign but can be due to a large thyroid cancer. Papillary thyroid carcinoma, follicular thyroid carcinoma, anaplastic thyroid carcinoma and primary thyroid lymphoma can all present as a goitre. The word goitre is from the Latin word guttur meaning throat. The normal thyroid gland measures 50mm in length by 20mm in width and 15mm in depth. The normal thyroid gland weighs about 15-20 grams.
As the thyroid enlarges it may cause symptoms from pressure or obstruction. Initially some patients complain of a pressure feeling in their neck or lower throat. Sometimes they are aware of a feeling of a lump in their throat, but most patients who complain of the feeling of a lump in their throat do not have an enlarged thyroid gland. The pressure feeling may result in coughing. As the thyroid enlarges it may stick out and be noticed by the patient. However, some enlarged thyroids do not stick out and at least initially are not obvious. I like to think of thyroids as either innies or outies, just like people describe tummy buttons (the umbilicus). One small difference is that some thyroids are both innies and outies. As the thyroid enlarges the sternal notch is lost. In fact, if you can not see a sternal notch expect to find an enlarged thyroid. As the thyroid enlarges it may cause swallowing problems from compression of the oesophagus or breathing issues from compression of the trachea. Breathing issues are most noticeable if someone exerts themselves (walking up stairs or up a hill) and when lying down. Snoring and obstructive sleep apnoea can be caused by a goitre. A goitre may cause a change in the voice. A very breathy voice is usually due to a vocal cord palsy and is a red flag that there may be cancer. With further enlargement of the thyroid there may be venous congestion and shortness of breath most noticeable when someone hangs the washing on the line. Most patients with goitres are euthyroid. Many patients with Hashimoto’s thyroiditis are hypothyroid. Some patients with goitre develop hyperthyroidism which is often proceeded by compensated hyperthyroidism (suppressed TSH and normal fT4).
In summary a goitre may cause:
- No symptoms

- A pressure feeling in the neck
- Feeling of a lump in the neck / throat
- A visible mass or be invisible
- Dysphagia
- Shortness of breath
- Orthopnoea
- Snoring
- Coughing
- Hoarseness
- Hyperthyroidism
What is Pemberton’s sign?
Pemberton’s sign is facial plethora when the arms are raised above the head. It was thought to be due to an enlarged thyroid descending into the thoracic inlet (the cork effect) obstructing veins, but a recent paper suggests it is due to the medial aspects of the clavicles compressing major venous structures within a narrowed thoracic inlet against an enlarged thyroid (the nutcracker effect). It is usually associated with compression of the trachea and shortness of breath. A positive Pemberton’s sign is facial plethora that occurs within one minute of raising the arms above the head.
What is stridor and what is the significance of the different types of stridor?
Stridor is simply noisy breathing. There are three different types of stridor:
- Inspiratory stridor: due to airway obstruction at or above the level of the vocal cords
- Biphasic stridor: due to airway obstruction at the level of the subglottis or trachea
- Expiratory stridor: due to airway obstruction of the small and medium sized bronchi as heard in asthma
Goitres that compress the trachea cause biphasic stridor.
Stridor may be present at rest or only noticeable on exertion.
To test for the presence of stridor ask the patient to turn their head slightly away (so they are not breathing on you), and to take a big breath in and out through their mouth.
What causes a goitre?
Two common causes of goitre are iodine deficiency and Hashimoto’s thyroiditis. Iodine is added to salt in many countries to help prevent goitre and this is especially important in those countries with endemic goitre. Iodine is also found in eggs, fish, seafood, chicken and beef liver. Poorly identified naturally occurring goitrogens are thought to cause most goitres.
Goitres are more common in females, with increasing age and in families with a history of goitre.
What is the natural history of a goitre?
Over time there is usually progressive enlargement of a goitre. A proportion of patients will develop hyperthyroidism. Pregnancy may result in rapid growth of a goitre resulting in airway obstruction.
When do I request an ultrasound and when to request a CT scan?
An ultrasound is good to assess thyroid tissue. If a patient has no symptoms or minimal symptoms and does not want surgery, then an ultrasound of the thyroid gives valuable information about the likelihood of thyroid cancer. A goitre frequently contains multiple nodules (a multinodular goitre) and it is important to ensure that the nodules are benign and not malignant. The best way to do this is to request an ultrasound scan. The nodules are graded as to their risk of malignany (tirads classification). Tirads 3 nodules >2.5cm, tirads 4 nodules >1.5 cm and tirads 5 nodules > 1cm require an ultrasound guided FNA
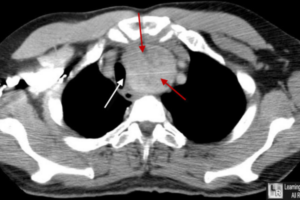
A CT scan is recommended anytime when you are unable to determine the inferior extent of the thyroid or when you suspect tracheal compression. A CT scan will image the whole goitre while ultrasound scan can only image the portion of the goitre that is in the neck. A CT scan will determine the degree of tracheal compression.


When to refer a patient with a goitre?
I recommend referral for a specialist opinion when the patient is symptomatic:
- Discomfort / pressure feeling in the neck
- Shortness of breath or stridor
- Dysphagia
- Hoarse voice
- Facial plethora when the arms are raised.
Or if there are any of the following:
- Rapid growth
- Lymphadenopathy
- Very large goitre
- CT scan shows tracheal compression
- Hyperthyroidism
Rapid growth, lymphadenopathy and a hoarse voice are all red flags and malignancy needs to be excluded.
Does thyroxine help to suppress the growth of a goitre?
The American Thyroid Association recommends not to prescribe thyroxine to suppress the growth of thyroid nodules. Thyroxine in most cases is ineffective at stopping or slowing the growth of thyroid nodules.
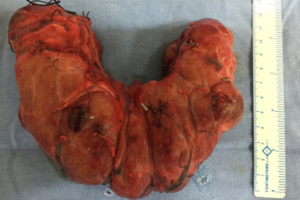
Surgery for a goitre
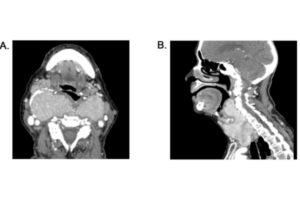
Surgery is recommended when the benefits outweigh the risks. Surgery is usually performed to relieve symptoms. In severe cases a goitre can cause life threatening compression of the trachea. The extent of tracheal compression is easily assessed with a CT scan. It is generally recommended that once the trachea is compressed by 50%, surgery should proceed. Patients can still be very symptomatic with less than 50% tracheal compression. Retrosternal extension is another indication for surgery. Surgery is recommended in patients with a positive Pemberton sign.
In most cases surgery is also recommended if there is thyroid cancer. Notable exceptions would be if there is advanced anaplastic thyroid carcinoma that is not totally resectable or for thyroid lymphoma.
Surgery is recommended for patients with hyperthyroidism and a goitre once the hyperthyroidism is under control. Patients with significant Grave’s orbitopathy usually require thyroidectomy before their eye disease comes under control. Patients with compensated hyperthyroidism (low TSH and normal fT4) frequently develop full hyperthyroidism and this is an additional indication for surgery when assessing a patient with a goitre.
Surgery is recommended for patients with as concomitant hyperparathyroidism and a goitre.
In summary thyroidectomy for patients with a goitre is indicated when:
- Significant symptoms
- Thyroid cancer
- Hyperthyroidism (control with medication first)
- Concomitant hyperparathyroidism
The extent of surgery depends on the extent of thyroid disease. For patients with enlargement of a single lobe of the thyroid, hemithyroidectomy is sufficient. Most patients with goitre have enlargement of both lobes of the thyroid and total thyroidectomy is indicated. Thyroxine replacement therapy is required following total thyroidectomy but not after hemithyroidectomy. The risks of thyroidectomy include injury to the recurrent laryngeal nerve resulting in voice change if unilateral (1%) and tracheostomy if bilateral (rare) and hypoparathyroidism (2%). Hypoparathyroidism (low adjusted serum calcium and low PTH) may be temporary or permanent. Injury to the external branch of the superior laryngeal nerve results in a change in pitch and volume of the voice. Bleeding, infection and an unsightly scar are other uncommon but well recognised complications.
What is the effect of a goitre on weight and fertility?
A goitre does not affect weight unless it is associated with hypothyroidism or hyperthyroidism. Most patients with goitres are euthyroid. There are important exceptions. Hashimoto’s thyroiditis may cause a goitre and is a common cause of hypothyroidism. Similarly, Grave’s disease may cause a goitre and is a common cause of hyperthyroidism. Plummer’s disease is a toxic multinodular goitre and patients with Plummer’s disease are hyperthyroid. If a patient has a goitre with compensated hyperthyroidism (suppressed TSH and normal fT4) there is a significant chance the patient will develop hyperthyroidism and this is one indication to operate. According to the American Thyroid Association most of the weight gain due to hypothyroidism is not due to fat accumulation but due to salt and water retention. Approximately 2-5 kg of body weight may be due to hypothyroidism.
Hypothyroidism and hyperthyroidism can negatively impact fertility-both the ability to become pregnant and the ability to carry a fetus to term. The presence of autoimmune antibodies, with or without hyper or hypothyroidism, can also negatively impact fertility.
Of course, after total thyroidectomy, the patient will need to take regular daily thyroxine medication. Provided the patient is euthyroid, this will have no impact on weight gain or fertility.
References
- Gregory W. Randolph. Surgery of the Thyroid and Parathyroid Glands. 3rd Elsevier, Philadelphia, PA, USA. 2021; chap 6: 53-69.
- Haugen BR, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26: 1-133.
- Grant EG, et al. Thyroid Ultrasound Reporting Lexicon: White Paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. J Am Coll Radiol 2015;12:1272-1279.